| |
| Med Sci (Paris). 34: 8–14. doi: 10.1051/medsci/201834f102.JTC-801 Suppresses Melanoma Cells Growth through the PI3K‑Akt‑mTOR Signaling Pathways Jing Li1,2 and Fei Huang3* 1School of Medicine, Shandong University, Jinan, Shandong, P.R. China 2Department of Dermatology, Shandong Provincial Third Hospital, Jinan, Shandong, P.R. China 3Department of Dermatology, Yucheng People’s Hospital, No.753, Kaituo Road, Yu Town, Yucheng 251200, Shandong, P.R. China |
Melanoma is considered as one of the most potentially fatal and aggressive malignancies. Due to the limited efficacy or drug resistance of the current targeted therapies of melanoma, developing new therapeutic drugs against new targets to effectively control tumor growth is greatly needed. In this study, the effect of JTC-801, a selective small-molecule antagonist of nociceptin receptor and analgesic agent, on a melanoma cell line, M14, has been studied. We demonstrate herein that JTC-801 could efficiently suppress the proliferation, migration and invasion capacity of the M14 melanoma cells, and induced a strong apoptosis. Importantly, our results provide the underlying molecular mechanism of these effects. JTC-801 cells regulate M14 cells by inhibiting the PI3K-Akt‑mTOR pathway. These results suggest that JTC-801 should be further studied in preclinical modes to establish whether it represents a potential small anticancer candidate drug against melanoma. Keywords: JTC-801, melanoma, PI3K, signaling pathway |
Melanoma is one of the most potentially fatal and aggressive malignancies, and its incidence continues to increase worldwide, resulting in an important socio-economic problem [1, 2]. The incidence of malignant melanoma from 1973 to 2002 increased by 270% in the United States; moreover, its incidence rate is approximately 10-fold greater in Caucasians than in other human populations [2, 3]. Though melanoma represents only about 3% of all skin cancers in the U.S., it accounts for about 75% of all skin cancer deaths [4]. Unlike other solid tumors, melanoma mostly affects young and middle-aged people. Until recently, the efficacy of the treatments available is limited. The traditional clinical therapy, such as surgery, radiation therapy and chemotherapy, have harmful side effects and are ineffective in advanced melanoma, particularly in patients with metastases. Other treatments, (not including immunotherapeutic approaches), such as the use of BRAF inhibitors, the mitogen-activated protein kinase (MAPK) signaling pathway targeted small-molecule inhibitors, that include vemurafenib and dabrafenib etc., have a limited clinical efficacy, due to the development of acquired drug resistance [5, 6]. Thus, there is a need to develop additional therapeutic drugs, to define new targets and strategies to effectively block tumor growth and improve long-term survival. JTC-801, [N-(4-amino-2-methylquinolin-6-yl)-2-(4-ethylphenoxymethyl) benzamide mono hydrochloride], is a specific antagonist of nociceptin receptors, also known as the nociceptin/orphanin FQ (N/OFQ) receptor (NOP). It includes the opioid receptor-like 1 receptor (ORL1), a member of the opioid receptor family with a potential role in modulating a number of brain functions, including instinctive behaviours and emotions [7]. Additionally, it is an orally active drug that provokes not only an antagonized nociceptin-induced allodynia but also has anti-hyperalgesic effects [8-10]. It has been reported that JTC-801 treatment reverses SPS-induced mechanical allodynia, thermal hyperalgesia, anxiety-like behaviour and hypocortisolism [11]. The Opioid systerm has been found not only as playing an important role not only in the nervous system but also in melanoma progression [12, 13]. However, until now, there is no report available to confirm the effect of the small-molecule JTC-801 on melanoma progression. In the present study, we found that JTC-801 effectively suppressed the proliferation, migration and invasion of M14 melanoma cells and induced their apoptosis. More importantly, we show a novel mechanism that underlies these effects based on the down-regulation of the PI3K-Akt‑mTOR pathway. Our results suggest that JTC-801 is a potential anticancer small molecular agent against melanoma. |
Reagents and antibodies The human M14 cells were obtained from The Chinese Academy of Sciences Shanghai cell bank (Shanghai, CHN). The cell culture medium RPMI-1640 was purchased from GE Healthcare Life Sciences (Logan, UT, USA). Fetal bovine serum, antibiotics and L-glutamine were from Life Technologies (Grand Island, N.Y.). Matrigel was from BD Biosciences (NJ, USA). JTC-801 was purchased from MedChemexpress (Monmouth Junction, USA). DMSO was obtained from Amresco (Solon, OH). Transwell chambers from Millipore (Temecula, CA); all antibodies are rabbit anti-human antibodies. Anti-AKT and phospho-AKT, -mTOR and -phospho-mTOR antibodies were purchased from Cell Signaling Technology (Beverly, MA); anti- GAPDH, -p-70s6k, -bcl-2, -bax, -active-caspase 3 antibodies and HRP-conjugated Goat Anti-Rabbit IgG were from Proteintech (Wuhan, CHN). The Annexin V-FITC/PI Apoptosis Detection Kit was from 4A Biotech (Beijing,CHN). CCK8-kit and trypsin were from Solarbio (Beijing,CHN). The BCA Protein Assay Kit and Protease Inhibitor Cocktail were from CWBIO (Beijing,CHN). The other reagents of molecular biology were from Sigma (St Louis, MO). Cell cultures The M14 cell line was supplied by the Cell Bank of the Chinese Academy of Sciences (Shanghai, China) and cultured in RPMI1640 supplemented with 10 % fetal bovine serum (FBS), 100 U/ml penicillin and 100 μg/ml streptomycin at 37 °C in an humidified atmosphere with 5 % CO 2 to the exponential phase of growth. M14 cells were washed twice with PBS before trypsinization. Media with FBS was added to stop trypsinization. After cells detachment and careful resuspension, cells were seeded in a 6-well plate to be at least 80% confluent with a good morphology. 10 µM JTC-801 (in DMSO X% ) was then added and the cells were cultured for 24 h. A dimethyl sulfoxide (DMSO) treatment was used as negative control (NC). Cellular proliferation assay Quantification of cellular proliferation was performed using a Cell Counting Assay Kit-8 according to manufacturer’s instructions. 1,000 cells were starved and plated into 96-well plates per well and cultured for 24 h.Then M14 cells were treated with 10 µM JTC-801 group or with 0.1 % DMSO (NC) group in triplicate. Proliferation rates were determined at 24, 48 and 72 h after treatment by measuring the absorbance (OD values) at 450 nm wavelength using a spectrophotometer (Bio-Rad, USA). The cells were treated with the CCK-8 reagent (10 µl/well) and incubated for another 1.5 h before detection. Experiments were performed at least three times and representative data are shown. Cell migration and invasion assay M14 cell migration and invasion were measured using the 8 μm pore, 6.5 mm polycarbonate transwell chambers containing 24-well inserts according to the manufacturer’s protocol. In cell invasion assay, Matrigel (BD Biosciences, USA) was diluted (1:6) in serum free-cold RPMI1640 which was thawed at 4 °C overnight. The upper chambers of transwell were then coated with 100 µl diluted Matrigel and incubated at 37 °C for 4 to 6 h to allow gelling. The gelled matrigel was then gently washed with 500 µl of pre-warmed serum-free RPMI1640. 600 μl full medium containing 10 % FBS were then added to the bottom chamber. M14 cells having been treated with JTC-801 or DMSO for 24h were harvested by trypsinization and resuspended in free-cold RPMI1640 at a density of 1×10 6 cells/ml. 100 µl of the cell suspension were seeded on the top chambers and incubated at 37 °C in a humidified incubator with 5% CO 2 for 24h for invasion evaluation. After removing the transwells from the 24-well plates, cells in the upper chamber were scraped off with a cotton swab. The cells attached to the lower surface of membrane were fixed in 4% paraformaldehyde at room temperature for 30 min and stained with 0.1 % crystal violet solution for 20 min. Cells were counted in five randomly selected fields (magnification, 200) for each transwell filter, and the mean number of cells per field for three independent membranes was calculated as the invasion index. A similar protocol was used for the cell migration assay but in absence of Matrigel. The migration time was allowed for 4-6 h. Flow cytometric apoptosis assay Cell apoptosis was evaluated using the PI and Annexin V-FITC staining method. M14 cells were incubated for 24 h with serum-free medium after treatment with JTC-801 or DMSO for 24 h. Then cells were collected by trypsinization (without EDTA), and washed twice with ice-cold PBS. Collected cells were then resuspended to 1-5×10 6 cells/ml in 1X binding buffer. 5 μl of Annexin V/FITC were added into 100 μl cell suspension for 5 min in the dark at room temperature. Cells were washed once and re-suspended in 10ul propidium iodide (PI). Following double staining, the cells were analyzed with a flow cytometer. The percentage of early apoptosis was calculated by counting the number of cells positive for annexin V and negative for PI. Flow cytometric plots were generated by FlowJo™ software (TreeStar, Ashland, OR). Three independent experiments were performed. Western blot analysis Western blot analysis was performed as described previously. M14 cells were harvested after treatment with JTC-801 or DMSO for 24 h and were lysed using ice-cold RIPA-based lysis buffer supplemented with protease inhibitors. The lysates were boiled for 5 min after protein concentration in the cell lysates was quantitatively measured with a BCA protein assay kit. The protein extracts of each sample were loaded about 20 μg protein / lane and resolved by 10 % SDS-PAGE. Then the gel was transferred to a PDVF membrane (Millipore, Bedford, MA, USA). Blocking of the PVDF Membranes was performed with 5 % (w/v) nonfat milk powder at room temperature for 1 h, and then was incubated with the primary antibody at 4 °C overnight. After that, the membranes were washed 3 times in TBS-T and were incubated with secondary horseradish peroxidase (HRP)-conjugated secondary antibodies at room temperature for 1 h. After washing 3 times with TBST, the chemiluminescent detection kit was utilized to immunodetection and then exposed to X-ray film. Experiments were performed at least three times. Relative densities of protein levels (ratio to GAPDH) of each group was measured by Quantity One (Bio-Rad company) software. Experiments were performed at least three times and representative data are shown. Statistical analysis Statistical analysis was performed with the SPSS statistical software (SPSS Inc., Chicago, IL, USA). Differences between the groups were compared using Student’s t test. All the values are represented as mean ± Standard Deviation (means ± SD). P<0.05 was considered as statistically significant. |
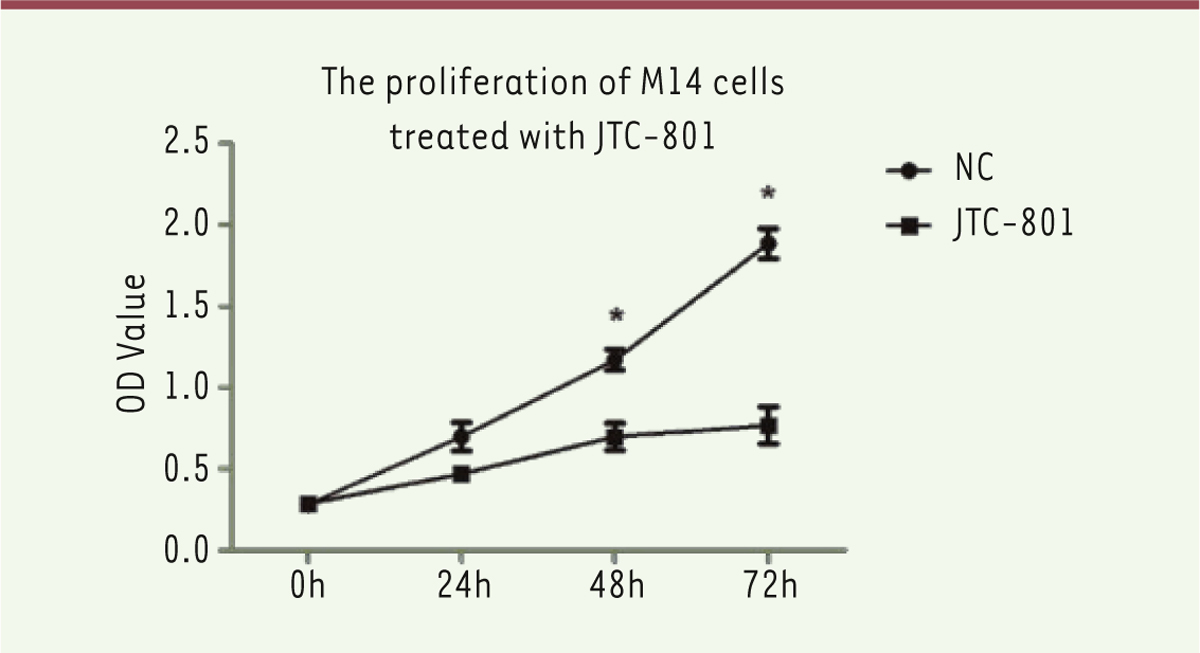
JTC-801 significantly suppresses M14 cells growth and proliferation In order to detect whether the small molecule JTC-801 may affect the melanoma biological behavior, a CCK8 assay was used to examine the impact of JTC-801 on the growth and proliferation of M14 cells, in which 4 time points were chosen (0, 24, 48, 72 h). The dose of JTC-801 (10 µM) was selected according to the results of a preliminary experiment. As shown in Figure 1, the absorbance values of the M14 cells at 48 and 72 h were significantly lower (P<0.05 for 48 and 72 h) than the untreated M14 cells. It indicates that the growth and proliferation ability are significantly decreased following JTC-801 treatment.
 | Figure 1. JTC-801 significantly reduced M14 cell growth and proliferation. Cell Counting Assay Kit-8 was performed to analyze the proliferation level of M14 cells. 24, 48 and 72 hours cell cultures were tested. JTC-801 (10 μM) treatment for 24h significantly inhibited M14 cells proliferation at all the time points analyzed (*, versus NC, P<0.05, Student’s t test). N = 3 for each group. |
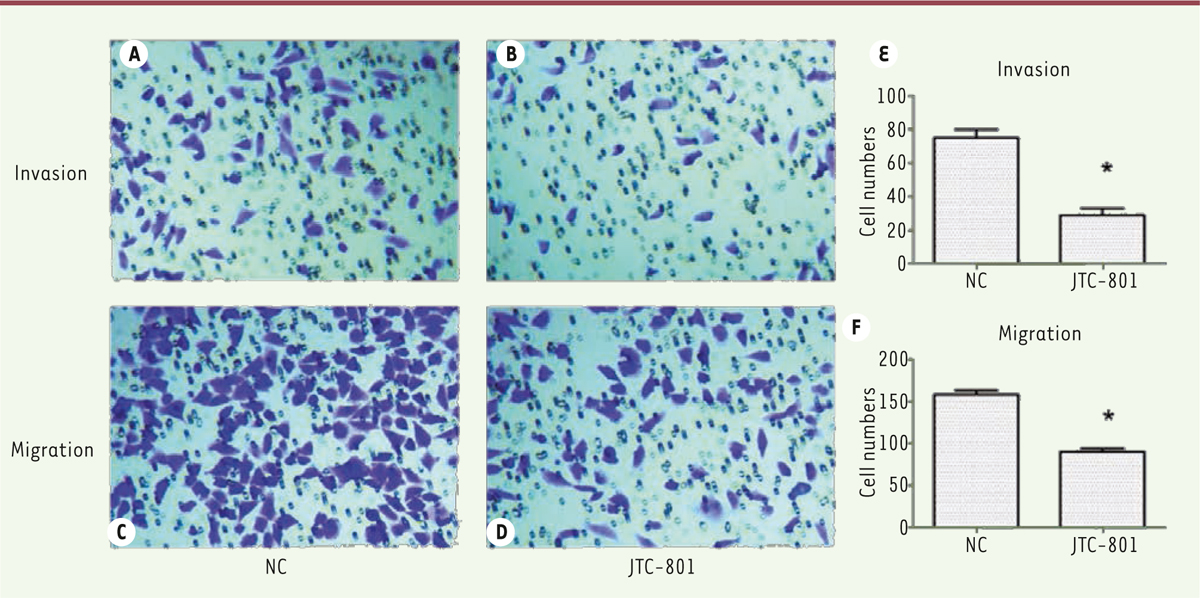
JTC-801 inhibits M14 cells migration and invasion A transwell migration and invasion assay (Transwell filters coated with Matrigel) was then performed to evaluate the effect of JTC-801 on the migration and invasion potential of melanoma cells. JTC-801 treatment showed around 2.3-fold decrease in the migration of M14 cells (P<0.05) compared with control (Figure 2B). The matrigel invasion assays showed that JTC-801 induced around a 2.4-fold reduction relative to the control M14 cells (P<0.05) (Figure 2A). These results indicate that JTC-801 can inhibit the migration and invasion capacity of M14 melanoma cells and, possibly, of other melanoma cells.
 | Figure 2. JTC-801 effectively inhibits M14 cell migration and invasion. A-D, M14 cell invasion and migration are shown after JTC-801 treatment (200 × magnification). E-F, histograms representing M14 cell invasion and migration after JTC-801 treatment. * P < 0.05 compared with NC group. N = 3 for each group. |
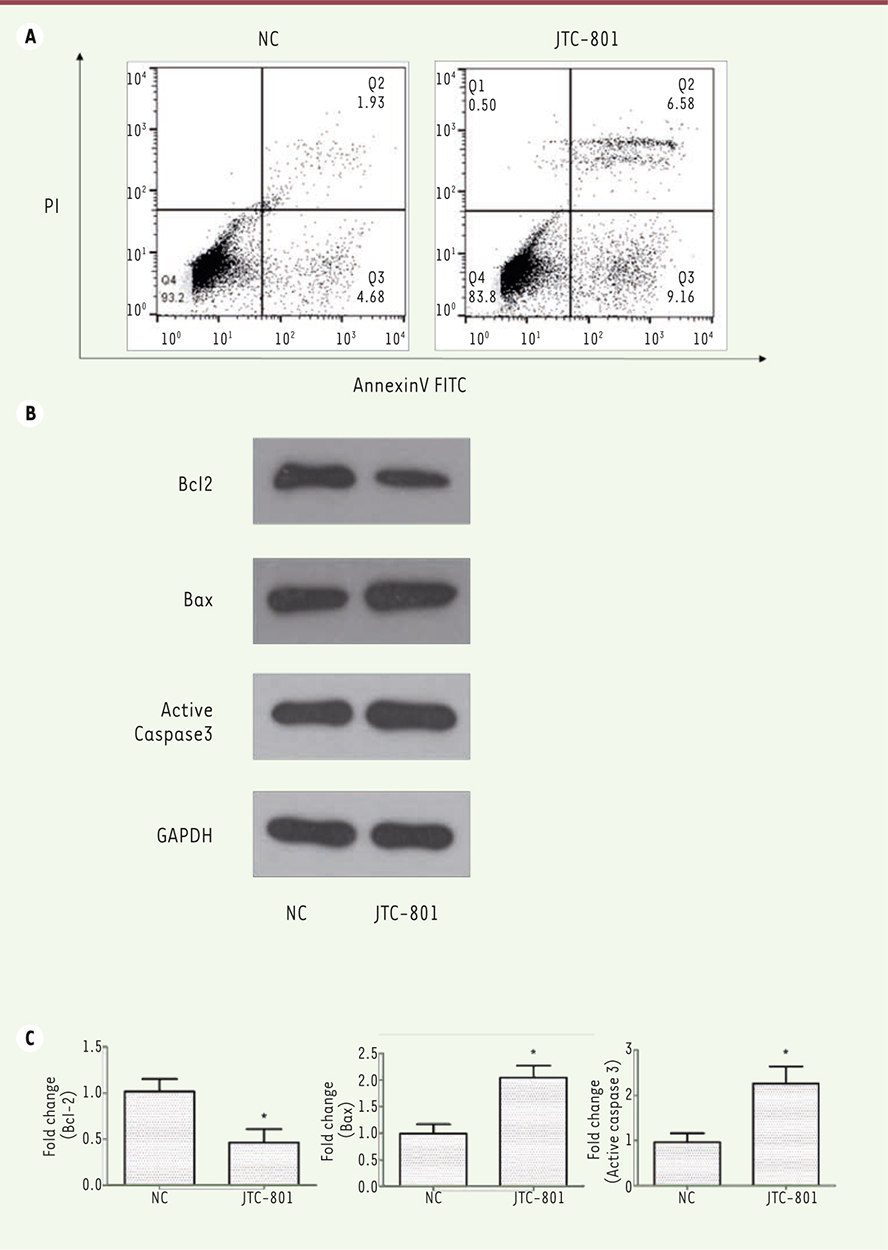
JTC-801 induces apoptosis of M14 cells To investigate if JTC-801 impacts the apoptosis of the melanoma cells, JTC-801-treated M14 cells were collected and analyzed with annexin V-FITC/PI double staining method on a flow cytometer. Treatments with JTC-801 distinctly enhanced the percentages of early and late apoptotic M14 cells (15.74% vs 6.61%) (Figure 3A).
 | Figure 3. JTC-801 induces apoptosis of M14 cells. A. JTC-801 enhances the percentages of early and late apoptotic M14 cells. The apoptosis-induced effect of JTC-801 in M14 cells was evidenced by an Annexin V/PI double staining assay. Representative images (left : untreated cells (NC); right, JTC-801 treated cells) were generated using the FlowJo™ software. B. Expression of the apoptosis-associated proteins Bcl-2, Bax and active casepase-3 as detected by Western-blot (representative images). JTC-801 increased the expression of apoptosis-inducing factors and decreased that of the anti-apoptotic protein (JTC-801 treatment for 24h). C. Histograms showing the differences (expressed as fold changes) observed in Westen-blot experiments shown in B (left panel, Bcl-2 ; middle panel, Bax ; right panel, active caspase-3; *, versus NC, P<0.05, Student’s t test). N = 3 for each group. |
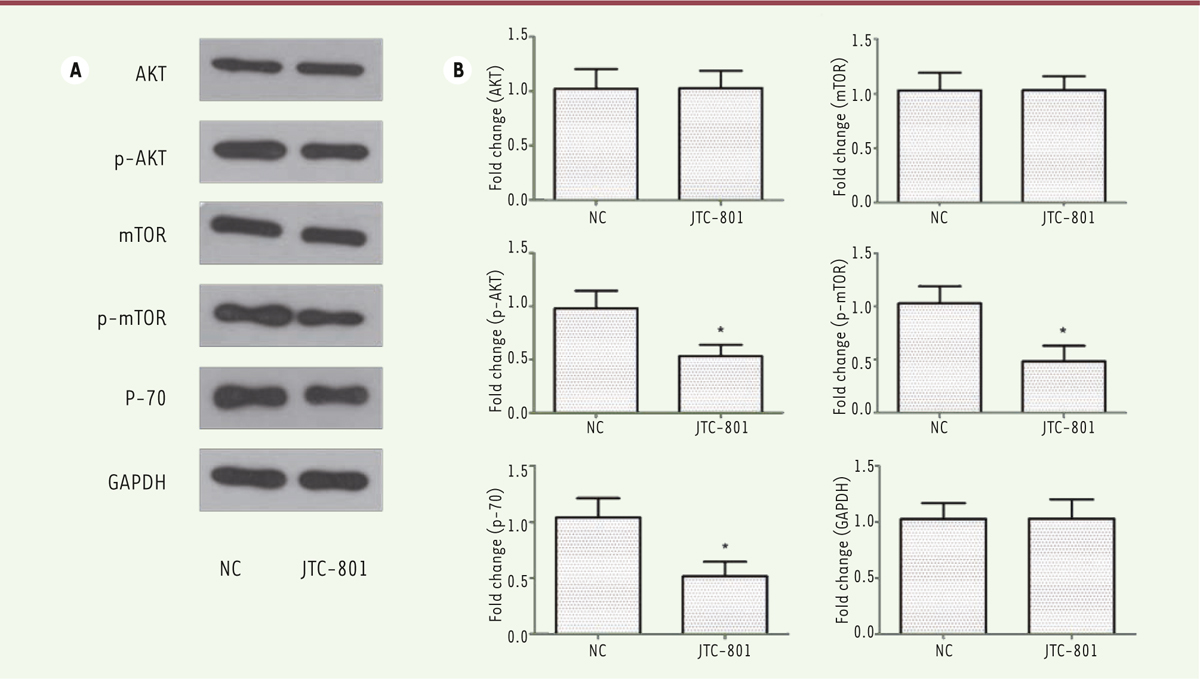
These observations led us to measure the expression level of apoptosis factors to assess whether they were activated during JTC-801 treatment. Thus, Western blot analyses were performed to evaluate the expression of the apoptosis-associated proteins Bcl-2, Bax and the apoptosis effector protein active caspase-3. As the other Bcl-2 family members, Bcl-2 suppresses apoptosis and promotes tumor progression; Bax promotes apoptosis and acts as a tumor suppressor. As shown in Figure 3B and C, the expression of Bcl-2 effectively decreased about 2-fold in the JTC-801 treated cells vs sham-treated cells. Simultaneously, both Bax and active caspase-3 expression dramatically increased to about two times as compared to the control values, which suggested that caspase-3 was activated and that more cells were induced into apoptosis. These data indicate that JTC-801 can induce the apoptosis of M14 melanoma cells. JTC-801 suppresses the activation of PI3K signaling pathways in M14 cells The phosphatidylinositol-3-kinase/protein kinase B (PI3K/Akt) pathway is a signaling pathway whose activation has been associated with cell proliferation, migration, and intracellular trafficking in many cancer cell types [ 14]. In addition, mammalian target of rapamycin (mTOR), an important downstream molecule of PI3K/Akt, regulates the serine/threonine kinase p70 S6 kinase (p70S6K), and this signal pathway has been proved to be a key mediator of proliferation and survival for melanoma [ 15, 16]. Thus, to explore whether this signaling pathway is involved in the decrease of the proliferation and migration of JTC-801-treated M14 cells, we performed a serie of western blot analyses. Figure 4 A and B shows that the treatment with JTC-801 provoked a significant decrease in the phosphorylation levels of Akt, mTOR and in the expression levels of p70S6K of about two-fold in the M14 melanoma cells, when compared with the control group. Taken together, our results suggest that JTC-801 regulates the biological behavior of M14 cells by down-regulating the activity of PI3K-Akt-mTOR pathway. In addition, it also confirms that the PI3K/Akt pathway is involved in the proliferation, invasion and survival of the cells of these melanoma cell line and possibly of tumor cells of patients with melanoma.
 | Figure 4. JTC-801 regulates the biological behavior of M14 cells through the down-regulation of the PI3K-Akt-mTOR pathway. A. Phosphorylation levels of Akt, mTOR and expression level of p70S6K in M14 cells after treatment with JTC-801 (Western-blots). B. Histograms showing the differences (expressed as fold changes) observed in Westen-blot experiments shown in A (*, versus NC, P < 0.05, Student’s t test). N = 3 for each group. |
|
Melanoma is one of the cancers with the fastest-rising incidence with a high mortality rate worldwide. In the present study, we have examines the anti-cancer effect of a small-molecule drug, JTC-801 on cells from a melanoma cell line, M14, and its underlying molecular mechanisms of action. Development of more effective small molecule agents is an urgent need to counter the acquired drug resistance and achieve desired therapeutic effects in melanoma, such as targeting MAPK, PI3K, and c-kit signaling pathways [17]. Recently, many small molecule compounds were designed and synthesized with the hope of exhibiting potent and efficient anti-cancer effects. For example, 50% of all cutaneous melanomas exhibit a Ras/Raf/MEK/ERK mitogen activated protein kinase (MAPK) signal transduction cascade with a mutationally activated BRAF molecule (BRAFV600E) [18]. The BRAFV600E targeting small-molecule inhibitors exert significant clinical therapeutic effect; however, a significant proportion of selective BRAF inhibitors leads to drug resistance in most clinical cases through the re-activation of the MAPK signaling via an ERK-dependent feedback in melanoma cells [5, 6, 19]. So it is urgently necessary to develop new drugs that target this pathway. JTC-801 is a small molecular antagonist of the ORL1 receptor which belongs to the noiciceptin receptor. The ORL-1 receptor is the fourth opioid receptor involved in neuropathic pain and inflammatory hyperalgesia. Although NOP shares a high sequence identity (~60%) with the ‘classical’ opioid receptors μ-OR (MOR), k-OR (KOR), and d-OR (DOR) [7], they have little or no affinity for opioid peptides or morphine-like compounds [20]. Thus, the anti-nociceptive effect of JTC-801 is not through opioid receptors [9]. Till now, most of the works reported about JTC-801 have been related to its analgesic effect in the nervous system. Interestingly, it has been reported that the opioid system include opioid receptor (KOR) agonists which are involved in the progression of melanoma and of other cancers. For example, kappa opioid receptor agonists act as anti-angiogenic factors in tumors [12, 13]. Whether JTC-801 has an anti-cancer effect in melanoma cells remains unclear and had not been investigated before our study. To assess the influence of JTC-801 on the viability and growth of M14 melanoma cells, the CCK8 assay was employed. Our results confirmed that JTC-801 could significantly suppress the growth and proliferation of melanoma cells (Figure 1). Metastasis is a leading cause of mortality and a a pivotal features of malignant tumors. One of the critical steps during tumor metastasis is the tumor cells migration and invasion. To investigate the effect of JTC-801 on M14 cells migration and invasion, transwell migration and invasion assays were performed. 10 µM JTC-801 treatment resulted in the suppression of not only the M14 cell migration but also of their invasion capacity. Apoptosis, also known as programmed cell death, is defined as a regulated cell death mediated by a strict intracellular program. The apoptotic process involves a cascade of proteolytic events accomplished mainly by a family of cysteine proteases [21], especially activated caspase-3, the major executioner of apoptosis. This process is regulated by Bcl-2 family members, among which Bax is known as a proapoptotic member that favors the leakage of apoptogenic factors from mitochondria, and Bcl-2 is an antiapoptotic member that negatively regulates this leakage [22, 23]. To evaluate if JTC-801 could induce apoptosis of M14 melanoma cells, an Annexin/PI double staining was performed. As shown in Figure 3A, 24 h treatment with 10 µM JTC-801 induced M14 cell apoptosis (detected at both early and late apoptotic stages). Western blot assays were then performed to decipher the underlying molecular mechanisms. JTC-801 could effectively downregulate BCL-2 about 2-fold compared to sham-treated cells and dramatically upregulate both BAX and active caspase-3 expression to about two times compared to the control values. These results provided a strong evidence that JTC-801 has an apoptosis-inducing capacity in M14 melanoma cells.Therefore, our study revealed that treatment with JTC-801 can efficiently impact the biological behavior of melanoma cells through the regulation of apoptosis. To our knowledge, the present study is the first to investigate the anti-cancer effect of JTC-801 on melanoma cells. In the present study, we also investigated the molecular mechanisms underlying the anti-cancer effects of JTC-801 on melanoma cells. PI3K/Akt signaling pathway is an important part of the intracellular signal transduction network and plays an essential role in proliferation, differentiation, angiogenesis, and metastasis of melanoma and other cancers [24, 25]. In addition, activation of the PI3K-Akt signaling pathway has been suggested to be a critical regulator mediating resistance to MAPK inhibitors [26, 27]. Hence, we focused our analysis on the PI3K-Akt pathway as the putative target of JTC-801-derived effect. Activated PI3K phosphorylation attracts proteins that contain a pleckstrin homology (PH) domain to the cell membrane and phosphorylates a number of effector proteins including Akt and mTOR [25]. The mTOR can phosphorylate Akt on the hydrophobic motif sites, impacting cell proliferation, metabolism and survival. The ribosomal protein S6 kinase (S6K) is a family of kinases, substrates of mTORC. It includes p70S6K, a 70-kDa cytoplasmic isoform involved in the regulation of translation [16, 28]. In the present study, western blot assays were performed to detect the phosphorylation levels of Akt, mTOR and the expression levels of p70S6K. Figure 4A and B shows that the treatment with JTC-801 reduced the activity of the PI3K-Akt-mTOR pathway by inhibiting Akt and mTOR phosphorylation in M14 melanoma cells subsequently leading to a significant downregulation of p70S6K. Our results demonstrate that JTC-801 modulates the biological behavior of M14 cells through down-regulating the activity of PI3K-Akt-mTOR pathway. In addition, they also confirm that the PI3K-Akt pathway is involved in proliferation, invasion and survival of M14 melanoma cells. Therefore, the present study reveals a new potential therapeutic application of the small molecular compound, JTC-801, as an anti-melanoma agent through the inhibition of the PI3K-Akt-mTOR signaling pathway. Further investigations are required to extend our observation to other melanoma cell lines and to evaluate this anti-tumor effect in relevant preclinical models and to determine whether there are other signaling pathways involved in this anti-tumor effect.. |
Conflict of interest statement Authors state no conflict of interest. |
1. MacKie RM, Hauschild A, Eggermont AM. Epidemiology of invasive cutaneous melanoma . Ann Oncol. 2009;; 20 Suppl (6) : :vi1.–7. 2. Rastrelli M, Tropea S, Rossi CR, Alaibac M. Melanoma: epidemiology, risk factors, pathogenesis, diagnosis and classification . In Vivo. 2014; ; 28 : :1005.–1011. 3. Gloster HM, Jr., Neal K. Skin cancer in skin of color . J Am Acad Dermatol. 2006;; 55 : :741.–60; quiz 61–4. 4. Narayanan DL, Saladi RN, Fox JL. Ultraviolet radiation and skin cancer . Int J Dermatol. 2010; ; 49 : :978.–986. 5. Sosman JA, Kim KB, Schuchter L, et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib . N Engl J Med. 2012; ; 366 : :707.–714. 6. Fedorenko IV, Paraiso KH, Smalley KS. Acquired and intrinsic BRAF inhibitor resistance in BRAF V600E mutant melanoma . Biochem Pharmacol. 2011; ; 82 : :201.–209. 7. Mollereau C, Parmentier M, Mailleux P, et al. ORL1, a novel member of the opioid receptor family. Cloning, functional expression and localization . FEBS Lett. 1994; ; 341 : :33.–38. 8. Shinkai H, Ito T, Iida T, et al. 4-Aminoquinolines: novel nociceptin antagonists with analgesic activity . J Med Chem. 2000; ; 43 : :4667.–4677. 9. Yamada H, Nakamoto H, Suzuki Y, et al. Pharmacological profiles of a novel opioid receptor-like1 (ORL(1)) receptor antagonist, JTC-801 . Br J Pharmacol. 2002; ; 135 : :323.–332. 10. Tamai H, Sawamura S, Takeda K, et al. Anti-allodynic and anti-hyperalgesic effects of nociceptin receptor antagonist, JTC-801, in rats after spinal nerve injury and inflammation . Eur J Pharmacol. 2005; ; 510 : :223.–228. 11. Zhang Y, Simpson-Durand CD, Standifer KM. Nociceptin/orphanin FQ peptide receptor antagonist JTC-801 reverses pain and anxiety symptoms in a rat model of post-traumatic stress disorder . Br J Pharmacol. 2015; ; 172 : :571.–582. 12. Boehncke S, Hardt K, Schadendorf D, et al. Endogenous mu-opioid peptides modulate immune response towards malignant melanoma . Exp Dermatol. 2011; ; 20 : :24.–28. 13. Yamamizu K, Furuta S, Hamada Y, et al. small ka, Cyrillic Opioids inhibit tumor angiogenesis by suppressing VEGF signaling . Sci Rep. 2013; ; 3 : :3213.. 14. Yuan TL, Cantley LC. PI3K pathway alterations in cancer: variations on a theme . Oncogene. 2008; ; 27 : :5497.–5510. 15. Karbowniczek M, Spittle CS, Morrison T, et al. mTOR is activated in the majority of malignant melanomas . J Invest Dermatol. 2008; ; 128 : :980.–987. 16. Magnuson B, Ekim B, Fingar DC. Regulation and function of ribosomal protein S6 kinase (S6K) within mTOR signalling networks . Biochem J. 2012; ; 441 : :1.–21. 17. Strickland LR, Pal HC, Elmets CA, Afaq F. Targeting drivers of melanoma with synthetic small molecules and phytochemicals . Cancer Lett. 2015; ; 359 : :20.–35. 18. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer . Nature. 2002; ; 417 : :949.–954. 19. Lito P, Pratilas CA, Joseph EW, et al. Relief of profound feedback inhibition of mitogenic signaling by RAF inhibitors attenuates their activity in BRAFV600E melanomas . Cancer Cell. 2012; ; 22 : :668.–682. 20. Butour JL, Moisand C, Mazarguil H, et al. Recognition and activation of the opioid receptor-like ORL 1 receptor by nociceptin, nociceptin analogs and opioids . Eur J Pharmacol. 1997; ; 321 : :97.–103. 21. Alnemri ES, Livingston DJ, Nicholson DW, et al. Human ICE/CED-3 protease nomenclature . Cell. 1996; ; 87 : :171.. 22. Yang J, Liu X, Bhalla K, et al. Prevention of apoptosis by Bcl-2: release of cytochrome c from mitochondria blocked . Science. 1997; ; 275 : :1129.–1132. 23. Fridman JS, Benedict MA, Maybaum J. bcl-X(S)-induced cell death in 3T3 cells does not require or induce caspase activation . Cancer Res. 1999; ; 59 : :5999.–6004. 24. Gustin JP, Karakas B, Weiss MB, et al. Knockin of mutant PIK3CA activates multiple oncogenic pathways . Proc Natl Acad Sci U S A. 2009; ; 106 : :2835.–2840. 25. Kwong LN, Davies MA. Navigating the therapeutic complexity of PI3K pathway inhibition in melanoma . Clin Cancer Res. 2013; ; 19 : :5310.–5319. 26. Atefi M, von Euw E, Attar N, et al. Reversing melanoma cross-resistance to BRAF and MEK inhibitors by co-targeting the AKT/mTOR pathway . PLoS One. 2011; ; 6 : :e28973.. 27. Gopal YN, Deng W, Woodman SE, et al. Basal and treatment-induced activation of AKT mediates resistance to cell death by AZD6244 (ARRY-142886) in Braf-mutant human cutaneous melanoma cells . Cancer Res. 2010; ; 70 : :8736.–8747. 28. Grove JR, Banerjee P, Balasubramanyam A, et al. Cloning and expression of two human p70 S6 kinase polypeptides differing only at their amino termini . Mol Cell Biol. 1991; ; 11 : :5541.–5550. |